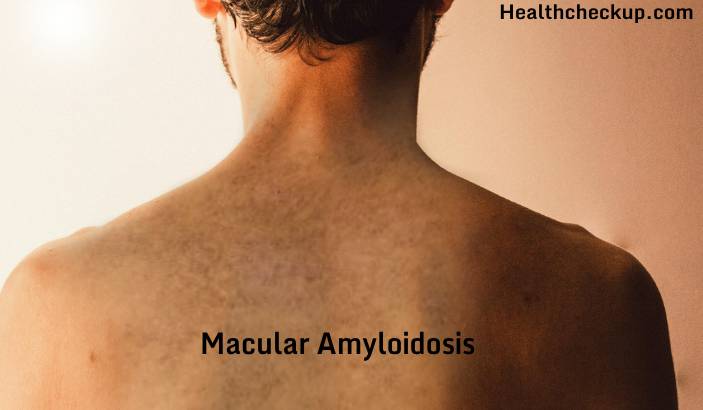
Macular amyloidosis is a skin condition characterized by the abnormal deposition of amyloid proteins in the skin, leading to hyperpigmented patches that can cause significant cosmetic concerns and discomfort. Although it is a benign condition, its chronic nature and the lack of a definitive cure make it a challenging disorder to manage.
What is Macular Amyloidosis?
Macular amyloidosis is a form of primary localized cutaneous amyloidosis (PLCA), a group of disorders characterized by the deposition of amyloid proteins in the skin without systemic involvement. The term “macular” refers to the flat, hyperpigmented spots or macules that are characteristic of this condition. These lesions are typically brownish or grayish in color and are commonly found on the upper back, chest, arms, and thighs.
Unlike systemic amyloidosis, which can affect multiple organs and be life-threatening, macular amyloidosis is confined to the skin and does not involve other parts of the body. However, the aesthetic impact and the potential for itching and discomfort make it a concern for many affected individuals.
Causes of Macular Amyloidosis
The exact cause of macular amyloidosis remains unclear, but several factors have been identified as potential contributors:
1. Genetic Predisposition
Genetics plays a significant role in the development of macular amyloidosis. The condition is more common in individuals of Asian, Middle Eastern, and South American descent, suggesting a hereditary component. Family history of the condition increases the likelihood of its occurrence, although the exact genetic mutations involved are not fully understood.
2. Chronic Friction and Scratching
Mechanical factors such as chronic friction, rubbing, or scratching of the skin have been implicated in the development of macular amyloidosis. The constant irritation of the skin is believed to stimulate the production and deposition of amyloid proteins, leading to the characteristic skin changes.
3. Environmental and Lifestyle Factors
Exposure to environmental factors such as sunlight and harsh weather conditions, as well as the use of certain skin care products, can exacerbate the condition. Additionally, lifestyle factors like poor skin hygiene or the use of abrasive clothing can contribute to the persistence and worsening of symptoms.
4. Autoimmune Mechanisms
Some researchers have suggested that macular amyloidosis has an autoimmune component, where the body’s immune system mistakenly targets its own tissues, leading to the deposition of amyloid proteins in the skin. However, this theory is still under investigation, and more research is needed to confirm its role in the condition.
Symptoms of Macular Amyloidosis
The primary symptom of macular amyloidosis is the appearance of hyperpigmented macules on the skin. These macules are usually:
- Brownish or Grayish: The color can vary depending on the individual’s skin tone and the duration of the condition.
- Flat and Asymptomatic: Unlike some other skin conditions, the lesions are typically flat and do not cause raised bumps or nodules.
- Itchy: Although not always present, itching (pruritus) can be a significant symptom, leading to discomfort and further scratching, which worsens the condition.
- Symmetrically Distributed: The macules often appear symmetrically on both sides of the body, particularly on the upper back, chest, and arms.
In some cases, the hyperpigmentation gradually spreads or darkens over time, leading to more noticeable and widespread skin changes.
Diagnosis of Macular Amyloidosis
Diagnosing macular amyloidosis typically involves a combination of clinical examination and histopathological analysis. The diagnostic process includes:
- Clinical Examination:
A dermatologist will examine the skin for characteristic features of macular amyloidosis, including the appearance, color, and distribution of the macules. The patient’s medical history, including any family history of similar skin conditions, will also be considered. - Skin Biopsy:
A skin biopsy is often performed to confirm the diagnosis. During this procedure, a small sample of affected skin is removed and examined under a microscope. The presence of amyloid deposits in the dermis confirms the diagnosis of macular amyloidosis. Special staining techniques, such as Congo red staining, are used to identify amyloid proteins. - Immunohistochemistry:
In some cases, immunohistochemistry is used to identify specific proteins associated with amyloid deposits, helping to differentiate macular amyloidosis from other types of cutaneous amyloidosis or pigmented skin conditions.
Treatment of Macular Amyloidosis
There is no definitive cure for macular amyloidosis, but several treatment options are available to manage symptoms and improve the appearance of the skin. Treatment strategies include:
- 1. Topical Treatments
- Corticosteroids: Topical corticosteroids can reduce inflammation and itching. However, long-term use should be avoided due to potential side effects such as skin thinning.
- Retinoids: Topical retinoids, such as tretinoin, helps to lighten hyperpigmented areas by promoting skin cell turnover and reducing pigment production.
- Calcipotriol: This vitamin D analog is sometimes used to manage hyperpigmentation and reduce amyloid deposits in the skin.
2. Laser Therapy:
Laser treatments, such as fractional laser therapy, have shown promise in reducing hyperpigmentation and improving the appearance of skin affected by macular amyloidosis. Laser therapy works by targeting the pigmented areas, breaking down the melanin, and stimulating collagen production.
3. Dermabrasion:
Dermabrasion is a procedure that involves the removal of the top layers of skin to reduce hyperpigmentation and smooth the skin’s surface. This treatment can be effective for some patients but require multiple sessions and has associated risks, such as scarring and changes in skin texture.
4. Phototherapy:
Narrowband ultraviolet B (NB-UVB) phototherapy has been used to treat macular amyloidosis by reducing inflammation and hyperpigmentation. This treatment involves exposing the skin to controlled amounts of ultraviolet light, which can help to fade the macules over time.
5. Systemic Treatments:
In more severe cases, systemic treatments such as oral retinoids (e.g., acitretin) may be prescribed. These medications work by reducing keratin production and slowing down the deposition of amyloid in the skin. However, systemic treatments are generally reserved for cases that do not respond to topical or procedural interventions.
Management and Prevention
Managing macular amyloidosis requires a combination of treatment and lifestyle modifications to prevent further irritation and worsening of the condition. Recommendations for management and prevention include:
- Avoiding Friction: Reducing friction and pressure on affected areas by wearing loose-fitting, non-abrasive clothing can help prevent the worsening of lesions.
- Sun Protection: Protecting the skin from excessive sun exposure can prevent hyperpigmentation from becoming more pronounced.
- Regular Skincare: Maintaining good skin care practices, including gentle cleansing and moisturizing, can help manage symptoms and improve skin texture.
- Regular Monitoring: Regular follow-up with a dermatologist can help monitor the condition and adjust treatment as needed.
Summary
Macular amyloidosis is a chronic skin condition characterized by the deposition of amyloid proteins in the skin, leading to hyperpigmented macules that can cause cosmetic and symptomatic concerns. While the condition is benign and does not involve systemic complications, managing its symptoms and appearance can be challenging due to the lack of a definitive cure. A combination of topical treatments, laser therapy, and lifestyle modifications can help improve the appearance of the skin and reduce discomfort.
I specialize in writing about health, medical conditions, and healthcare, drawing extensively from scientific research. Over the course of my career, I have published widely on topics related to health, medicine, and education. My work has appeared in leading blogs and editorial columns.