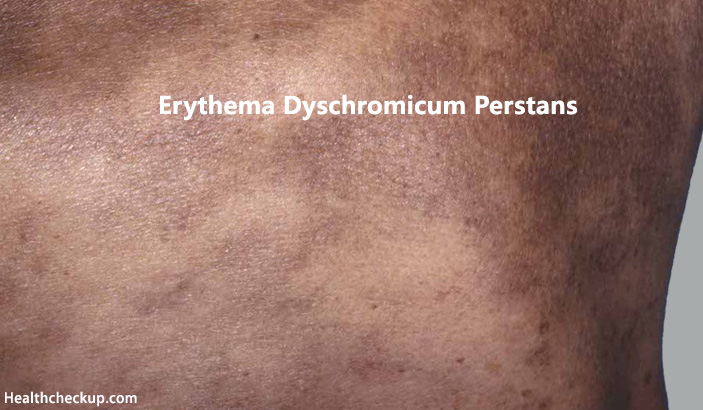
Greek eruthēma oreruthainein means ‘Be Red’, while ‘Dyschromic’ is a general term used for any discoloration of skin or nail in medical science. Hence, Erythema Dyschromicum Perstans (EDP) also known as Ashy Dermatosis refers to a persistent local redness of the skin. It is actually a chronic form of erythema multiforme- in which the relapses recur so persistently that the eruption is almost permanent.
It can be signified as an uncommon form of dermatosis with presenting feature of hyper-pigmented ash-grey coloration of the dermis with the formation of macule varying in size and shape occurring in a uniform gesture involving the face, extremities, more commonly in the trunk.
Initially the patches are present as grey or blue-brown circumferential or irregularly shaped macules, generally non elevated having a slightly raised reddish margination. However, a little hypersensitivity like irritation and itching may occur. Because EDP is an uncommon disease of the skin, it is important to consider other skin diseases that may resemble Erythema Dyschromicum Perstans, such as infectious diseases (i.e. leprosy), reaction to drugs, post inflammatory hyperpigmentation and also darker coloration of skin.
Erythema Dyschromicum Perstans Causes
Though it is a condition of unknown etiology- multiple tropical, physiological and systemic factors play key role to its development like age (more common in adulthood for having a gradual occurrence), radiation injury, exposure to ammonium nitrate, cobalt or CFC etc. It is often described as a variant of lichen planus. As the histopathological features of these both are almost the same. The following theories are often presented as the cause for EPD:-
- Genetic predisposition was thought to be an acute reason for the development of EPD. However, the recent methodology doesn’t support it.
- Toxic effects of chemicals such as ammonium nitrate or barium sulphate, chloride
- Whipworm (Trichuristrichiura) infestation
- Parasitic infections of different kinds.
- Adverse effect of drugs and medications
- Individual’s symptomatic or idiopathic hypersensitivity.
Erythema Dyschromicum Perstans Symptoms
With vast range of variety in occurrence and modulation of the condition, it is very hard to specify any symptomatic nature exactly. But, as of clinical study database, it is represented as follows:
- Formation of numerous asymptomatic slate grey macules
- Gradual progression of size, number and shape of macules
- Distribution over face, neck, upper trunk and extremities
- Lesions start usually over right side of a part (e.g. neck, trunk – most commonly in the neck) and new lesions appear gradually to involve other body areas
- Multiple, round to oval, very small sized (0.5-5 cm) bluish grey colored macules over cheeks, chin, neck, upper chest and back, abdomen, and limbs
- Lesions show distinct minimally elevated erythematous (reddish) borders
- Hair, nails, teeth, palms, soles, mucous surfaces and systemic examination could probably be normal. However, a biopsy can reveal otherwise.
Erythema Dyschromicum Perstans Differential Diagnosis
It should be kept in mind that, various other skin conditions may represent similar features of Erythema Dyschromicum Perstans (EPD). As these are also associated with resulting in origination of discolored skin patches. These conditions are:-
- Lichen planus pigmentosus (EPD may be a variant of this disorder)
- Multiple lesions of fixed drug eruption
- Postinflammatory hyperpigmentation
- Urticaria pigmentosa
- Incontinentia pigmenti
- Pinta
- Leprosy
- Hypersensive idiopathic eruptive hyperpigmented macules, occurring irrespective of histological manifestation.
- Tropical rash
Erythema Dyschromicum Perstans Diagnosis
This is why, recommended diagnostic method is to perform a skin biopsy including a complete hemogram, blood biochemistry, urinalysis, and stool examination for intestinal parasites. The indicators for these complications like focal changes of moderate compact hyperkeratosis, epidermal thinning, basal cell degeneration, melanin incontinence, lympho-histiocytic infiltration in the upper dermis etc should be found for a positive case of EPD. As for coloration and margination for early lesions- minor vacuolar degeneration of the basal layer is a significant characteristic, while pigmentary incontinence with dermal melanophages in usually found in case of established patches.
Erythema Dyschromicum Perstans Treatment
While agents unspecified and ranging within a great probability from certain medications, radiographic contrast, pesticides, infection with parasites to even HIV, the cause of this skin disease as of today remains unknown. As a result, there is no distinguished cure for EDP. And thus, the treatment of EDP is largely unsatisfactory and remains challenging.
Unfortunately, EPD is rather resistant to currently available treatments. It may persist unchanged for years although some cases eventually clear up by themselves. However, the individual’s healing factor can be boosted by topical corticosteroids, oral antibiotics, vitamins, isoniazid, chloroquine, griseofulvin, exposure to ultraviolet radiation, IR therapy, LASER therapy, chemical peels. Besides these, only clofazimine and dapsone have been considered of some therapeutic benefit. Although treatment with clofazimine is not considered curative and the effect is quite poor, it has been a successful treatment in many cases.
But, as an adaptive step, prescribing topical tacrolimus ointment (0.1% – twice daily) has proven great influence. All the skin lesions usually disappear during following 3 months. However, this methodology is yet under research.
To Conclude
Erythema Dyschromicum Perstans – a local lesion, a disease of the dermis with unknown cause, a complication without proper treatment. It is a distinct and somewhat controversial cutaneous eruption that may be best regarded as a form of lichen planus or lichen planus actinicus and may persist for years. EDP has a benign outcome, with most complaints relating to cosmetic issues.
A lesion is always considered as a warning for those who suffer and to those who treat. The most common cause of a skin lesion is an infection on or in the skin. But it can vary from a systemic infection, an infection throughout the body, genetic predisposition, or even to a birthmark. And skin cancers including melanoma, basal cell carcinoma, and squamous cell carcinoma often start as changes to the skin. They can be new growths or precancerous lesions changes that are not cancer but could become cancer over time. So, irrespective of the cause and result – a lesion should be treated properly without any delay.
Medically Reviewed By