Blood Cancer – This word can arouse fear and anxiety in everybody’s mind. The word “Cancer” itself is sufficient enough to describe intensity and severity of a disease.
A lot of lifestyle changes like cigarette smoking, physical inactivity, junk food and improper diet, lack of sleep, exposure to environmental toxins and chemicals and sedentary habits are known to be some of the reasons why people might develop cancer. A renowned textbook of medicine also calls night-shift duties as Carcinogenic.
Cancer is certainly a disease which has multiple causes and multiple types too. It has emerged to be a global problem and the number of cancer cases has simply increased over the last few years. Cancer is also a leading cause of death worldwide.
What Exactly Happens In Blood Cancer?
As an example, when our mouth is injured due to some reason, healing occurs and normal cells re-grow. The healed tissue is just as it was earlier.
Sometimes, instead of the normal tissues, abnormal cells grow and multiply taking place of normal cells. These cells are very notorious! They start replacing the other normal cells also and go on multiplying and spreading to other parts. This abnormal cell growth and multiplication are called Cancer.
When these abnormal cells grow at some place within the body, they cannot be seen and signs and symptoms appear much later. Often, signs and symptoms are also treated as a transient disease, not expecting it to turn out into cancer.
Cancer of blood or of some organ of the body is diagnosed when more serious signs and symptoms start appearing. This is the sole reason why cancers, when diagnosed, are frequently at a much later stage when cancer has already become widespread.
The term blood cancer includes cancers of the bone marrow, blood circulation and lymphatic system. Hemopoiesis is a process by which normal blood cells are formed in the bone marrow.
In the bone marrow, two types of stem cells are responsible for production and maturation of normal blood cells. The two types are
| Myeloid Progenitor Cells | Lymphoid Progenitor Cells |
| These cells are responsible for production and maturation of
● Thrombocytes (platelets) ● Monocyte/ Macrophages ● Eosinophil ● Neutrophil ● Basophil |
These cells are responsible for production and maturation of
● Natural killer cells (large granular lymphocyte) ● T-lymphocyte ● B-lymphocyte/ Plasma cells
|
Types of Blood Cancer in Adults
Basic terms about blood cancer will help you understand the article better
1. Leukemia – A blood cancer in which there is an abnormal increase in number of immature white blood cells. In leukemia, either the myeloid or lymphoid cells of bone marrow affected.
2. Lymphoma – In this type of blood cancer, there is abnormal, excessive production of lymphocytes. B-lymphocytes and T-lymphocytes are found in lymph tissues. Therefore, cancer of B or T lymphocytes causes enlargement of the lymph tissues forming tumors.
3. Myeloma – It is cancer of plasma cells or B-lymphocytes.
| Type of Blood Cancer and Description | Causes and Features | Blood Cancer Staging |
| Myelodysplastic syndrome (MDS)
Commonly seen in people above 50 years of age.
This is a type of leukemia-related blood disorder in which blast cells (immature blood cells) fail to mature in the bone marrow.
Mutations in the bone marrow stem cells are a possible mechanism behind failure of blood cells to mature.
Myelodysplastic syndrome can develop into Acute Myeloid Leukemia later.
|
Causative Factors
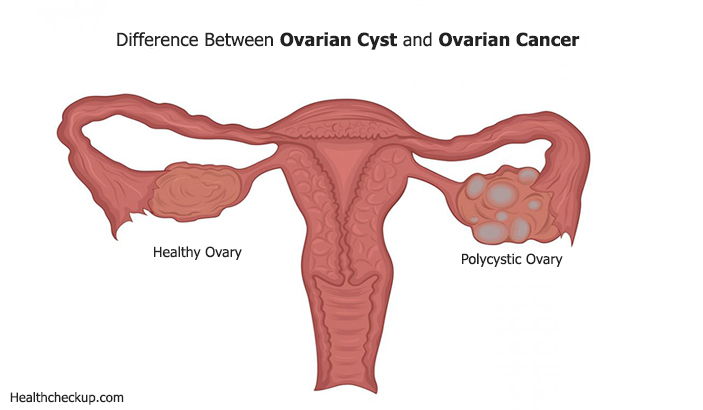
● MDS can be primary –having no identifiable cause. ● Secondary to receiving chemotherapy or radiotherapy for illnesses like ovarian cancer or Hodgkin’s lymphoma. ● MDS can also be genetic in origin. ● Other causes include exposure to tobacco, pesticides and heavy metals like lead or mercury. ● Children with Down’s syndrome are at a risk of developing MDS. ● Family history of sideroblastic anemia or Fanconi’s anemia is additional risk factors.
Clinical Features: Pancytopenia or low levels of: ● Red blood cells – symptoms of anemia like fatigue, chest pain or breathlessness ● White blood cells – increased risk of having infections ● Platelets – bleeding or subcutaneous hemorrhage Most of the patients remain asymptomatic and anemia, neutropenia or thrombocytopenia is identified on routine check-up. |
The French-American-British classification of MDS is:
1. Refractory anemia (meaning anemia which does not respond to treatment)
2. Refractory anemia with ringed sideroblasts
3. Refractory anemia with excess of blasts
4. Refractory anemia with excess blasts in transformation.
5. Chronic myelo-monocytic leukemia
|
| Acute Myeloid leukemia (AML)
AML is seen commonly in adults in contrast to acute lymphoblastic leukemia which is commonly seen in children.
There is a rapid growth of abnormal blood cells within the bone marrow. Eventually, these abnormal leukemic cells replace normal cells of the bone marrow.
Acute leukemia progresses rapidly and if left untreated, it is fatal.
|
Causative Factors
● Exposure to chemotherapy and radiation ● Cigarette smoking ● Exposure to benzene (benzene and its derivative compounds are carcinogenic. Benzene exposure is commonly found as an occupational hazard.). ● Genetic factors and family history are equally responsible for causing AML. ● Down’s syndrome is associated with a risk for developing Acute Myeloid Leukemia.
Clinical Features Abnormality at the level of myeloid cells causes lack of red blood cells, majority of white blood cells and platelets. Lacks of cells cause: ● Anemia, fatigue, shortness of breath – RBCs ● Increased risk of infection – WBCs ● Easy bruising or bleeding from slight trauma – platelets. Leukemic cells tend to infiltrate gum tissues and therefore swelling of gums is seen. Enlarged spleen and lymph nodes. Bone tenderness is present in maximum number of patients. Presence of Auer rods on bone marrow aspiration examination is diagnostic for acute myeloid leukemia.
|
French-American-British classification of acute myeloid leukemia is:
M0 – minimally differentiated myeloblastic leukemia
M1 – myeloblastic leukemia without maturation
M2 – myeloblastic leukemia with maturation
M2baso – myeloblastic leukemia with basophil blasts M3 – hyper-granular promyelocytic leukemia
M3 variant or hypo-granular bilobed promyelocyte
M4 – myelomonocytic leukemia
M5 – monocytic leukemia
M5a – poorly differentiated monocytic leukemia
M5b – well differentiated monocytic leukemia
M6 – erythro-leukemia
M7 – Acute megakaryoblastic leukemia |
| Chronic Lymphocytic Leukemia (CLL)
In this type of blood cancer, there is excessive production of B-lymphocytes.
This condition affects people above the age of 50 years and is more common in males than in females.
Acquired hemolytic anemia is often the first presentation and also a complication of CLL.
|
Causative factors:
● Genetic mutations are responsible for CLL ● Exposure to Agent Orange (a pesticide and a chemical) ● Viral infections ● Blood transfusions ● Exposure to ionizing radiation
Clinical Features: ● Signs and symptoms of anemia ● Lymph node enlargement bilaterally including enlarged tonsils ● Enlargement of spleen and liver ● Bleeding manifestations because of reduced platelets ● Increased risks of infections ● Bone pain and joint pains
|
Rai’s staging for Chronic Lymphocytic Leukemia:
Stage 0 – absolute lymphocytosis (>15,000/ cumm) without anemia, thrombocytopenia, lymphadenopathy and enlarged liver and spleen.
Stage I – absolute lymphocytosis with lymphadenopathy
Stage II – absolute lymphocytosis with enlarged spleen or liver or both
Stage III – absolute lymphocytosis with anemia with/without hepato-splenomegaly and lymphadenopathy.
Stage IV – absolute lymphocytosis with thrombocytopenia (Platelets <100,000 cumm)
|
| Chronic myeloid leukemia (CML) or Chronic granulocytic leukemia
This type of blood cancer belongs to myelo-proliferative group of disorders.
There is an increase in abnormal myeloid cells in the bone marrow.
CML occurs commonly at the age of 50-60 years.
|
Causative Factors
● Bone marrow abnormality due to presence of Philadelphia chromosome is the cause. ● Exposure to radiation ● Chronic exposure to benzene and its derivatives.
Clinical Features: ● Grossly enlarged spleen with pain in left side of the abdomen. ● Enlarged liver ● Poor appetite, weight loss and night sweats are some common constitutional symptoms. ● Anemia, fatigue, tachycardia and shortness of breath because of anemia. ● Bruising and hemorrhage from least trauma because of low platelets. ● Vitamin B12, uric acid and serum LDH are elevated.
|
Stages of CML
Chronic phase
Accelerated phase
Acute phase or blast crisis
|
| Polycythemia rubra Vera (PRV)
This rare blood cancer belongs to the myelo-proliferative group of disorders in which there abnormal, excessive production of red blood cells by the bone marrow.
About 2 in 100,000 patients have this type of blood cancer. However, it occurs in people above 60 years of age.
This happens because myeloid cells in the bone marrow multiply rapidly.
In PRV, because of increase in red blood cells, blood becomes thick or viscous and because of reduced flow, risk of thrombosis increases.
Although there in an increase in RBCs, they are hypo chromic and microcytic.
|
Causative Factors
In PRV, since the myeloid cells are affected, you may have increase in number of platelets and white blood cells also. ● In maximum number of patients, this blood cancer occurs due to a mutation in a protein called the JAK2 protein. ● In a normal person, JAK2 protein regulates production of RBCs, WBCs and platelets.
Clinical features: ● Because of increase in red blood cells, the skin has a reddish appearance (ruber) ● Headache, dizziness, visual disturbances ● Tinnitus, difficulty in hearing ● Constipation and occasionally GIT-bleeding ● Palpitations, chest pain or even heart failure ●High systolic blood pressure ● Fatigue and weight loss. ● Enlarged spleen is a seen in about 75% cases ● Enlarged liver is seen in about 50% of cases ● Peptic ulcers, chronic myeloid leukemia and myelofibrosis are common complications (presence of scar tissue in the bone marrow) In spite of signs and symptoms, PRV is usually diagnosed on a routine checkup. |
|
| Myelofibrosis
Myelofibrosis is a rare type of blood cancer in which there is extensive scarring of the bone marrow because of which there is reduced production of blood cells.
This blood cancer belongs to myelo-proliferative group of blood disorders.
It usually affects people above 50 years of age.
Patients with myelofibrosis tend to develop acute leukemia rapidly which is fatal.
|
Causative Factors
● Mutation in the JAK2 gene is the cause for myelofibrosis. ● Patients with thrombocythemia and polycythemia rubra vera usually develop myelofibrosis at a later stage. ● Chronic exposure to benzene. ● Exposure to radiation.
Clinical features: ● Features of anemia are commonly seen. ● Easy bruising and bleeding due to low or abnormal platelets ● Fever and bone pain are common ● Enlarged liver and spleen. ● There is an over-production of defective platelets. ● Formation of blood cells outside the bone marrow (extra-medullary erythropoiesis) causes formation of tumors and swelling.
|
Types of myelofibrosis are:
Idiopathic – having no known or identifiable cause.
Secondary – to infiltration from infections or other cancers, chemicals, toxins and radiation.
|
| Essential Thrombocythemia (ET)
Essential thrombocythemia is a rare blood cancer belonging to the myeloproliferative group of disorders.
In this condition, there is an over-production of platelets by the bone marrow (more than 10,000,000 per ul of blood)
It affects both males and females equally of 50-60 years of age.
|
Causative factors:
● JAK2 kinase gene mutation is responsible for this condition.
Clinical features: ● Elevated platelet count and WBC count and reduced RBCs on routine blood investigation. ● Bleeding due to dysfunctional or abnormal platelets. ● Formation of clots or thrombosis of blood vessels is a common complication due to increase in platelets. ● Headache, dizziness and visual disturbances ● Nausea and vomiting ● Enlarged spleen
|
|
| Hairy Cell Leukemia (HCL)
This type of blood cancer belongs to lympho-proliferative group of disorders. Hairy cell leukemia is a variant of chronic lymphocytic leukemia.
It affects males more than females in the age group of 40-60 years.
In HCL, there is excessive production of B-lymphocytes which obstructs growth and maturation of other WBCs, RBCs and platelets. |
Causative factors:
There are no specific, known causes for HCL. ● People engaging in agriculture or gardening. ● Chronic exposure to herbicides ● Exposure to ionizing radiation
Clinical features: ● Signs and symptoms due to low RBCs, WBCs and platelets are seen. ● Enlargement of spleen. Splenic rupture is a common complication. ● Peripheral lymph node enlargements ● Hair-like cytoplasmic projections in bone marrow and spleen.
|
|
| Non-Hodgkin’s Lymphoma (NHL)
NHL affects B and T lymphocytes.
It affects people in the age group of 15-30 years.
|
Causative factors:
● Klinfelter’s syndrome is associated with a risk of having NHL. ● Autoimmune diseases like rheumatoid arthritis and SLE ● Exposure to chemicals ● Exposure to radiation and chemotherapy ● HIV and Hepatitis C infection ● H.Pylori infection ● Epstein Barr virus infection ● Family history of NHL
Clinical features: ● Enlarged lymph nodes ● Constitutional symptoms like fever, weight loss and night sweats ● Itching of skin ● Metastasis to the brain causes altered sensorium, confusion, personality changes and even seizures |
Staging of NHL:
Staging is done based on the group of lymph nodes affected
Stage 1 – one group of lymph nodes
Stage 2 – two or more groups of lymph nodes above or below the diaphragm
Stage 3 – lymph nodes affected on both sides of the diaphragm
Stage 4 – involvement of other organs like lungs, liver, brain
|
| Hodgkin’s Lymphoma (HL)
In this variety of lymphoma, there is involvement of lymph tissues and is characterized by presence of Reed-Sternberg cells in the lymph nodes.
It affects people in the age group of 20-40 years. It is more common in males than in females.
|
Causative factors:
● Epstein Barr Virus is the commonest causative factor for Hodgkin’s lymphoma. ● HIV infection ● Family history of Hodgkin’s lymphoma ● History of having non-Hodgkin’s lymphoma ● Hepatitis C virus infection
Clinical features: ● Enlarged lymph nodes ● Fever, weight loss and night sweats ● Features of anemia ● Alcohol consumption causes pain at lymph nodes affected. ● Cough, shortness of breath and chest pain due to involvement of mediastinal lymph nodes ● Itching of skin ● Enlarged liver and spleen ● Non-specific back pain and bone pain ● Nephritic syndrome is a common complication. |
Hodgkin’s lymphoma can be of 4 types:
1. Lymphocyte predominant HL
2. Mixed cellularity HL
3. Lymphocyte depletion HL
4. Nodular sclerosing HL
Staging for Hodgkin’s Lymphoma is similar to Non-Hodgkin’s Lymphoma.
|
| Multiple myeloma
This is a cancer of B-lymphocytes or plasma cells. There is excessive production of B-lymphocytes or plasma cells which eventually forms a tumor outside the bone and weakens it. It also obstructs formation and maturation of other blood cells.
The plasma cells form a mass within the bone marrow or above the bone.
This blood disorder commonly affects elderly individuals around 60 years of age or more.
|
Causative factors:
Exact cause for multiple myeloma is not known. Certain risk factors have been identified: ● Family history ● Exposure to chemicals and radiation ● Obesity ● Alcohol consumption ● Certain genetic mutations ● Acute or chronic renal failure
Clinical features: ● Bone pain and tenderness. Persistent pain is indicative of fractures. ● Anemia because of infiltration of bone marrow ● Infections due to low immunoglobulin and other white blood cell types ● Bleeding tendencies because of low platelet count ● Neurological symptoms like sensory loss and paraplegia
|
Staging of multiple myeloma:
Stage I – beta 2-microglobulin <3.5 and albumin >3.5
Stage II – neither stage I nor stage III values
Stage III – beta 2-microglobulin >5.5
|
Plenty of above mentioned blood cancers don’t have an alarming presentation and they are usually diagnosed on a routine blood checkup.
This is the reason why screening has been given so much importance keeping disease prevention in view. Secondly, diagnosis of cancer at an early stage can be treated and the disease progress can be stopped.
More recently, that people have started to educate themselves and understand more about cancer and they definitely take steps to prevent it.
Maintaining a healthy lifestyle goes a long way not just in preserving health but also in disease prevention.
Medically Reviewed By
Dr. Himanshi is a Homoeopathic consultant and currently working as a lecturer in Post-graduate faculty of Homeopathy, Parul University, Vadodara. Completed BHMS and MD in Homeopathy in January 2018 and also has a clinical experience of about 6 years. Personal interests include reading, spending time with family and traveling.